Provided by Field Reimbursement Managers:
-
HIPAA compliant support throughout the reimbursement process
- In depth education on using the Coherus Solutions™ portal to track your patients information on billing, coding, and coverage and reimbursement rates
- Assistance with reimbursement issues
- Educational support on:
- Treatment approval process
- Patient assistance programs
- National and local payer policies
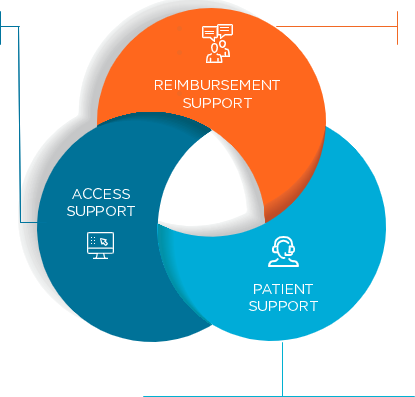
Through Financial Assistance Programs:
-
The Coherus Solutions™ Co Pay Assistance Program
- The Patient Assistance Program (PAP)
- Alternative funding options through independent foundations
Provided by Patient Access Specialists:
-
Product specific benefit verification
- Coverage, coding, and reimbursement education
- Prior authorization (PA) services*
- PA and claims appeal processes*
- Proactive monitoring of independent foundations to identify available funds
- Product replacement support